1. Introduction
ccording to the Institute of Medicine (IOM; Bootman 2000), between 44 000 and 98 000 patients die every year in the US as a result of preventable medical errors and another million or so are injured (Bootman 2000; Kohn et al. 2001). These findings led to an initiative by the US Federal Government to improve patient safety and create a more cost-effective healthcare system (Porter and Teisberg 2006; Shortell and Singer 2008;Singer et al. 2003). The US Center for Medicare and Medicaid Services (CMS) also attempted to reduce medical errors and improve patient safety, while holding hospitals accountable (Leape and Berwick 2005;McGlynn et al. 2003). Their quality measures relate to certain medical conditions that are particularly prone to preventable medical errors, which are available for 98% of US hospitals (nearly 4700) and are a widely used benchmark for the quality of care provided by a hospital to its patients and thus used to quantify performance (Department of Health and Human Services (HHS), 2011). They also encourage competition between hospitals (Arrow et Shojania et al. 2001), but we used the CMS measures to assess quality-of-care performance in our study (CMS database; HHS 2011).
2. a) Theoretical context
To satisfy the need to provide high-quality and safe patient care and reduce costs, hospitals must establish efficient organizational traits and suitable leadership styles within the context of either modern or lean management systems.
There has been limited success of the major initiatives so far (Leape and Berwick 2005;Singer and Shortell 2008). As Porter (2009) noted: "The US healthcare system remains largely the same as it was a decade ago with no convincing approach to changing the unsustainable trajectory of the system, much less to offsetting the rising costs of an aging population and new medical advances." Implementing successful systems and processes is still a challenge for hospitals. They are aware of the need to, but struggle with the choices available (Boyer et al. 2012;Proudlove et al. 2008), not least because of a lack of studies in the area. Hence the rationale behind the present study which aims to identify specific drivers of performance in terms of quality of care (HHS, 2011) and investigate the interrelationships between management systems, organizational traits and leadership.
Studies have been conducted into lean management practices in healthcare, particularly organizational learning, standardized processes, tools and continuous improvement (Boyer and ). There may be observational bias in studies with limited population sizes that focus on one type of hospital (Kane 2006), which may mask the effects of management systems, organizational traits and leadership on performance outcomes.
This study focused on factors from four variables -lean management, modern management, organizational traits, and leadership -using the publicly available CMS quality-of-care measures (HHS 2011) for nearly 4700 hospitals. These factors constituted the dependent variable for measuring overall performance, and consisted of factors relating to acute myocardial infarction, heart failure, pneumonia and the surgical care improvement project (HHS 2011).
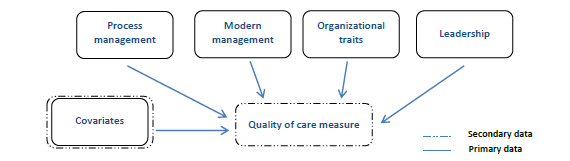
Independent variables were collected by surveying 597 hospitals related to four key criteria (Figure 1): lean management principles, modern management principles, organizational traits and leadership characteristics. An empirical census survey has been conducted to test the construct shown in Our study examined both lean and modern management in the hospital environment. Modern management ideas, originally from Alfred Sloan at General Motors, were adapted by General Electric and others until the 1990s (Lean Enterprise Institute 2010; Womack 2010). This style of management promotes organizations with departments, clear managerial authorities, vertical delegation, and a top-down approach; managers are developed through formal education and decisions are made far from the point of value creation. Its practices are not viewed favourably by lean management organizations (Womack 2010), the principles of which are based on the Toyota production system (Liker, 2004). The lean management philosophy focuses on horizontal flow of value across a hospital and on improving processes towards a perfect patient experience.
This study treated modern and lean management as separate factors and used explanatory factor analysis and principal component extraction to combine them analytically.
3. c) Organizational traits
Firm, well-rounded organizational traits in hospitals correlate positively with effectiveness, efficiency and innovation (Dalton et al. 1980;Robinson and Luft 1985). We investigate whether organizational traits have any impact on hospital performance.
4. d) Transformational and transactional leadership
Our analysis was based on empirical evidence of the influence of transformational and transactional characteristics on quality outcomes. According to leadership theory, hospital performance and quality of care strongly depend on leadership ( 2005). No significant difference was found between responders and non-responders (p = 0.1654-0.8753).
5. c) Covariates
Covariates were selected for within-hospital factors, including the type of hospital (cv3; acute care, acute care veterans administration, or critical access) and organizational structure (subsidiary or stand-alone) (CMS 2012). External factors included the number of years respondents had been employed by their hospital.
6. d) Data analysis
Confirmatory factor analysis (Dyer et al. 2005;Thompson et al. 2004) was used for each of the independent variables to account for common variance. Internal reliability and validity of dichotomous items were checked using Cronbach's alpha (Bland and Altman 1997;Gliem and Gliem 2003). All components had reliability alpha > 0.8, indicating good internal consistency. Our quality-of-care measure (dependent variable and a number between 0 and 1) was non-linear, requiring logit transformation (Ashton 1972;Jaeger 2008), and we used all-subset multiple linear regression (Belsley 1980; Myers 1990).
To select the statistical model, we applied forward elimination and a nominated alpha of 0.05. To account for errors in selection, we used an 80% sample of our dataset. The remaining 20% were used to assess the model's accuracy (mean absolute percent error; mean error) and bias (Hocking and Leslie 1967).
7. III.
8. Results
9. a) Survey data
We received 186 questionnaires with all questions answered. We split them 80/20 (147/29) to create and validate the model and check for bias and errors. No correlations exceeded 0.47 or triggered further investigations (Thompson et al. 2004). After checking the individual effects of items separately, with an absence of differences in results, we ran the best subset model creation algorithm for all items (Myers 1990; Belsley et al. 1980).
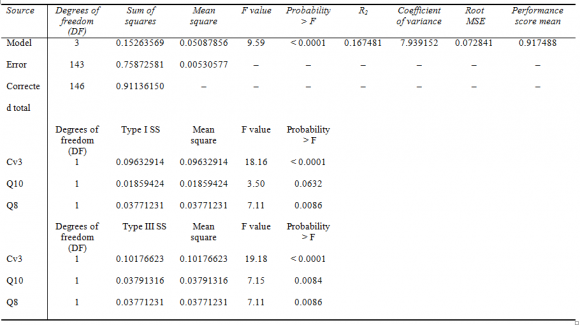
For the four all-subset models (for all components investigated), significant items were shown and ranked according to adjusted R 2 (coefficient of determination), showing that the best-fitting model includes covariate cv3 (type of hospital), and two independent variables, q8 (modern management system factor Managers often have to revisit/rework problems because they did not determine the root cause) and q10 (lean management factor Managers are responsible for cross-functional activities in addition to their own functional areas).
Covariate cv3 is important in the quality-of-care performance of hospitals, whereby acute-care hospitals are associated with positive outcomes. Table 1 shows that independent variables q8 and q10 both relate negatively to hospital performance. Table 2 shows the R 2 to be 0.167, meaning that 16.7% of the variation in quality-of-care performance among hospitals can be explained by a model consisting of variables cv3, q10 and q8. Terms for which estimates are followed by the letter B are not uniquely estimable.
10. Year ( )
We theorized that lean management has an impact on hospital quality-of-care performance. However, Table 1 shows that items q10 and q8 have a significant, negative impact on hospital performance. We found no evidence that organizational traits or leadership have any impact. None of the items in our best model pertaining to leadership were found to be significant (alpha 0.05).
Our results remain robust after a series of checks on our all-subset multiple linear regression model. We controlled for other hospital-level covariates such as hospital ownership (proprietary, voluntary nonprofit and government), the state in which it is located, and the type of organization (investor owned and for profit, non-government and non-profit, and state and local government), but found no significant influence on performance. Therefore, we did not include any of these covariates in our best subset model list.
Controlling for states showed that being located in Virginia, Washington and Wisconsin had a negative influence on performance. At the hospital level, we checked whether performance was influenced by belonging to a chain or a self-standing organization, and found a moderate negative effect (comparing means), but this did not influence our best model selection.
We also tested the impact of some process improvement factors on performance, whether they hospitals are "owned" by a focused, one-purpose process improvement department or handled by a department with additional tasks (e.g. a qualitymanagement department). We found a negative effect for situations where process improvements are handled by departments with additional tasks, but this was not strong enough to change our model. We also tested the impact of resource allocation in terms of FTEs (full-time equivalents) towards process improvement initiatives and found a negative influence of low FTEs (0 and 0.01-0.75 FTEs), and a small positive effect if 0.76-4.00 FTEs are allocated.
None of the above robustness checks resulted in changes to our model that best predicts variation in hospital performance (Table 1). We also checked for robustness of our model using a proportion of the results that were withheld in order to assess bias and accuracy as mean absolute percent error and mean error (Hocking and Leslie 1967). Thus, all of our results proved the robustness of our model and the presence of significance of determination.
IV.
11. Discussion
Our study tests how factors pertaining to lean management, modern management, leadership and organizational traits impact on quality-of-care performance outcomes in US hospitals, using CMS data from 2010 (CMS 2011) and survey information from 2011. We found that management system factors do influence hospital performance, but not to the expected extent.
Current management systems are often ineffective for managing the growing demand for care (Porter 2009; Porter and Teisberg 2007). We found one factor of modern management (Womack 2009) that negatively impacts on hospital performance, providing a potential area for improvement, namely Managers often have to revisit/rework problems because they did not determine the root cause. Our finding supports Womack's (2009) claim that without the right mindset and tools to solve the root cause of problems, sustainable improvements are not possible (Liker 2004;Womack 2002;Womack 2008). Hospitals need to empower their employees to resolve such issues.
We found no positive influence of lean management on performance, but the item Managers are responsible for cross-functional activities in addition to their own functional areas was negatively related. This finding should be interpreted with care, because the phrasing of the question might have led respondents to assume that efficiency increases if clear functionalities are in place (rather than that managers have to deal with both functional and cross-functional activities). These findings do not concur with those of Birkmeyer Another challenge is to identify organizational traits that drive performance. We found no evidence that such traits have any impact, although one covariate had a moderate negative impact when the improvement initiative is part of a department and not an independent unit. These results are inconsistent with research on the influence of organizational characteristics (Aiken et al. 1994(Aiken et al. , 2002 Unlike most studies that investigate individual aspects of hospital performance, we derived an overall construct using an all-subset multiple linear regression (Belsley et al. 1980;Myers 1990). This method accounts for correlations, Variance Inflation Factor (VIF) numbers and residual sums of squares, and eliminates the influence of co linearity. There are limitations, however, such as over-fitting the model, and selecting the wrong variables due to correlated proxies. These results should be interpreted with care, therefore, especially because logit transformation of performance score was used to achieve linearity of data.
There are several limitations associated with survey-based research (Dillman 2007;Rea and Parker 2005). In our case, responses were drawn from only one respondent from each hospital (Dillman 2007; Rea and Parker 2005), and certain states were misrepresented or under-represented (namely, Alaska, Hawaii and Idaho). Again caution is advised when generalizing about these findings.
A further limitation was that we measured four factors using questions derived from multiple sources (Bass and Avolio 1994;Eagly et al. 2003;Greene 1975;Hirst et al. 2004;Pawar and Eastman 1997;Wofford-Vicki et al. 1998). These should be validated in the hospital context. Furthermore, the questionnaire had only been used twice previously, within manufacturing environments, calling for further research within the healthcare and other industries.
This study contributes to our understanding of the influence of selected factors on hospital performance. It highlights the need for ongoing research in operations management, strategy and healthcare delivery, particularly with respect to management systems (modern vs lean), hospital type (acute vs critical care), transformational and transactional leadership, and organizational characteristics. A better understanding of the drivers of hospital performance will increase the chance of affordable, quality healthcare in the USA.
12. Global

| There were 30 non-responders who were contacted by | items), pneumonia (7 items) and the surgical care | |
| phone and tested non-response bias by one demographic question, six organizational traits questions and one continuous improvement methodology question (Alreck and Settle 1995; Connolly and Connolly 2005; Dillman 2007; Rea and Parker | improvement project (b) Survey data | |
| Survey data were collected from 597 hospitals. | ||
| The questionnaire consisted of Likert-scale, open-ended and categorical-scale questions on specific | Year | |
| management and organizational issues, hospital | ||
| indicators (such as inpatient days, triage, discharge, | ||
| 1998). Transactional leadership is driven by "management-by-exceptions" and contingent rewards (Bass and Avolio 1994); critics claim that it does not consider the human aspect of work and fails to empower people (Bass and Avolio 1994). Both styles have drawbacks, but hospitals employing either tend to perform better than hospitals that use neither. A few studies reveal that combining transformational and transactional traits can produce even better outcomes than applying them separately (Eagly et al. 2003; Greene 1975; Hirst et al. 2004; Pawar and Eastman 1997; Wofford-Vicki et al. 1998). The survey also addressed hospital indicators such as inpatient days, triage, discharge, turnover rates, Apache scores, hospital background and improvement methodologies. The secondary dataset derived from the CMS database was only applied to hospitals for which we also had survey data. II. Materials and Methods a) Hospital performance data Hospital data were compiled from publicly | ? 9 questions on lean management (adapted from Womack 2009). ? 9 questions on modern management (adapted from Womack 2002; 2008) ? 6 questions on organizational traits addressing how well the hospital functions effectively, efficiently and innovatively, and why patients and associates are satisfied with its performance (adapted from Great Place to Work 2012; NIST 2011; Womack 2009) ? 12 question on leadership (adapted from the multifactor leadership questionnaire (Avolio and Bernard 2004; Bass and Avolio 1994), Baldrige Criteria for Performance Excellence (Hutton 2000), transformational leadership questionnaire (TLQ-turnover rates, 1997). The final questionnaire comprised: | Global Journal of Management and Business Research Volume XVI Issue II Version I ( ) A |
| available Government records (HHS, 2011; CMS 2010) | LGV, Alban-Metcalfe and Alimo-Metcalfe 2000) and | |
| for 4697 hospitals from the American Hospital | a publication by McGuire and Kennerly (2006)). | |
| Association, State Hospital Associations, and the | Questionnaires were emailed to hospital | |
| Institute for Healthcare Improvement (IHI, 2010). The | managers across 48 states (Rea and Parker 2005) | |
| performance indicators relate to serious health | between July and October 2011. A total of 597 were | |
| conditions associated with preventable medical errors: | returned, with different response rates from different | |
| acute myocardial infarction (8 items), heart failure (4 | states (e.g. none from Rhode Island and 38 from Texas). |
| Parameter | Hospital type | Estimate | Standard error | t value | Probability > |t| |
| Intercept | - | 0.9913095284 B | 0.03524225 | 28.13 | < 0.001 |
| Cv3 | Acute care VA | 0.0000000000 B | - | - | - |
| Cv3 | Acute care | 0.0559908743 B | 0.01278468 | 4.38 | < 0.001 |
| Cv3 | Critical access | 0.0000000000 B | - | - | - |
| Q10 | - | -0.0164634543 | 0.00615886 | -2.67 | 0.0084 |
| Q8 | - | -0.0160801169 | 0.00603145 | -2.67 | 0.0086 |
| VA, veterans' administration. | |||||